您当前的位置: 首页

Currently cancer is usually diagnosed when tumours are already developed requiring,often significant,treatment to remove them and prevent further growth.However,a research team at the University of Cambridge will receive over£1.5m from Cancer Research UK over the next six years to investigate how the immune system evolves,targets and kills cancer cells as tumours are developing.They hope by detecting the trigger point when our own body starts to recognize cancerous cells,it may help find away to spark our own immune system into action so it kills cancer cells before tumours can even begin.This could vastly reduce the amount of treatment people diagnosed with cancer require,which can often have significant side effects.The pioneering work could benefit millions of cancer patients before the disease becomes life-threatening or spreads.Dr Heather Machado is leading ateam of scientists at the Department of Pathology,looking at the body‘s immune system‘s ability to fight cancer.Dr Machado’s work on Tcells–part of the immune system which fight infection and disease,including cancer–will provide an insight into how long before adiagnosis these cells recognize and respond to cancer.The study will specifically examine how Tcells respond to cancer when they first recognise and respond to atumour in the kidneys or the liver.The breakthrough study has the potential to unlock the mystery as to how our immune cells work to fight cancer.Dr Machado said:“Using mutations that naturally accumulate in each of our cells as we age,we can essentially build afamily tree of T-cells,and this family tree has information about when T-cells met cancer for the first time.This research is only now possible as aresult of advancements in DNA sequencing technology.“This research has the potential to give an entirely new perspective on the role of the immune system in cancer progression,findings that we hope to use to further improve lifesaving cancer immunotherapies.”Her aim is to see if they could lead to specific immunotherapy treatments and ways of detecting the cancer earlier.She added:“Most cancers are diagnosed years or decades after early tumour development,which can often be too late.Our methods will allow us to go back in the cancer’s timeline to understand the immune response in these early stages of cancer development.Beyond improving immunotherapies,we hope that this understanding helps us detect cancer earlier,at stages where survival rates are much higher.”The body’s immune system is the first line of defence against cancer but previously it has been difficult to observe this early response in humans.Dr Machado will use genome sequencing which determines the genetic makeup of an organism to study how atumour and the immune cells co-evolve over the course of tumour development. 查看详细>>
来源:剑桥大学 点击量: 0
“As complex living systems,we likely have trillions upon trillions of tiny nanoscopic holes in our cells that facilitate and regulate the crucial processes that keep us alive and make up who are,”says Marija Drndi?,a physicist at the University of Pennsylvania who develops synthetic versions of the biological pores that“guide the exchange of ions and molecules throughout the body.”The ability to control and monitor the flow of molecules through these pores has opened new avenues for research in the last two decades,according to Drndi?,and the field of synthetic nanopores,where materials like graphene and silicon are drilled with tiny holes,has already led to significant advances in DNA sequencing.In apaper published in Nature Nanotechnology,Drndi?and Dimitri Monos,her longtime collaborator at the Perelman School of Medicine and Children’s Hospital of Philadelphia(CHOP),presented anew kind of nanopore technology with the development of adual-layer nanopore system:a design that consists of two or more nanopores,stacked just nanometers apart,which allows for more precise detection and control of molecules like DNA as they pass through.“With current platforms,when molecules like DNA are placed on the nanopores it’s sort of like spaghetti in apot:tangled and difficult to work with,let alone guide through asingle hole,”Monos says.Typically,researchers need to use proteins to unwind and straighten it,which,while effective,has many limitations due to degradation that leads to reduced sensitivity and shorter operational lifespans,he says.“But with this new design,”Monos says,“we’re essentially guiding molecules through two coupled nanopores in the material,providing acontrolled,smoother passage of molecules and making them easier to detect and analyze.”The researchers call this new platform GURU to denote that“it’s aguided and reusable,”way to study molecules,which confers afew key benefits,most notably,the ability to better assess the length and conformation of molecules as they pass through the nanopores. 查看详细>>
来源:美国宾夕法尼亚大学 点击量: 0
An assistant professor of medicine(rheumatology,allergy and immunology)at Yale School of Medicine(YSM)and Yale Center for Clinical Investigation Scholar,Chock researches maternal health and offspring outcomes among patients with rheumatic diseases.She is interested in utilizing large clinical datasets to support her work.Recently,Chock received funding from the Yale Center of Excellence in Regulatory Science and Innovation-Food and Drug Administration Office of Women’s Health to develop the use of AI to remove barriers to diagnosing and addressing autoimmune diseases in women.In aQ&A,Chock discusses why early diagnosis of autoimmune conditions is important,how machine learning can help,and her hopes for the future of artificial intelligence in medicine.Why is it important to diagnose autoimmune diseases in women?In the U.S.,approximately 50 million people are affected by autoimmune diseases,and the number is rising.The incidence of systemic lupus erythematosus,for instance,has nearly tripled in the U.S.over the last 40 years.Eighty percent of individuals affected by autoimmune diseases are women,and many of these diseases have systemic implications,meaning they involve multiple organs.Sex differences influence the onset and severity of these diseases,which can be fatal.Timely diagnosis and treatment can ensure optimal outcomes.Tell us about your novel machine-learning approach to improve diagnostics in this area.Many patients are referred to arheumatologist because they receive apositive antinuclear antibody,or ANA,test result.An ANA test is avery common blood test that screens for autoimmune diseases,particularly lupus and scleroderma.But this test is not perfect.Not all individuals who test positive for ANA have or will develop autoimmune diseases.Since many people test positive for ANA and are referred to arheumatologist,the wait lists for these specialists are long.This is adisservice to patients who do have or end up developing an autoimmune disease because their prompt evaluation and care are delayed.In addition,getting apositive test result can cause unnecessary fears among patients,especially if they have to wait along time to see aspecialist.I am working in collaboration with Na Hong,PhD,instructor of Biomedical Informatics and Data Science at YSM,to use artificial intelligence software to efficiently extract data from electronic health records.Using amachine-learning tool,we’ll identify patients who test positive for ANA and are at risk of developing autoimmune diseases.We’ll also identify patients who have an ANA and don’t develop autoimmunity.All of this is done confidentially in asecure environment.Once we have these two groups of people,we’ll find data points—such as lab test results or medications—in the electronic health records within the Yale ealth system that indicate whether apatient has additional risk factors to develop lupus,scleroderma,or another autoimmune disease down the road.Once we gather this information from the electronic health records,we’ll apply artificial intelligence software to create an algorithm to help us identify ANA-positive patients who are at higher risk for developing an autoimmune disorder. 查看详细>>
来源:耶鲁大学 点击量: 0
The vision of people with arare inherited condition that causes them to lose much of their sight early in childhood was 100 times better after they received gene therapy to address the genetic mutation causing it.Some patients even experienced a10,000-fold improvement in their vision after receiving the highest dose of the therapy,according to researchers from the Perelman School of Medicine who co-led the clinical trial published in The Lancet.“That 10,000-fold improvement is the same as apatient being able to see their surroundings on amoonlit night outdoors as opposed to requiring bright indoor lighting before treatment,”says the study’s lead author,Artur Cideciyan,a research professor of ophthalmology and co-director of the Center for Hereditary Retinal Degenerations.“One patient reported for the first time being able to navigate at midnight outdoors only with the light of abonfire.”A total of 15 people participated in the Phase 1/2 trial,including three pediatric patients.Each patient had Leber congenital amaurosis as the result of mutations in the GUCY2D gene,which is essential to producing proteins critical for vision.This specific condition,which affects less than 100,000 people worldwide and is abbreviated as LCA1,causes asignificant amount of vision loss as early as infancy.Improvements were noticed quickly,often within the first month,after the therapy was applied and lasted for at least 12 months.Observations of participating patients are also ongoing.Three of six high-dosage patients who were tested to navigate amobility course in varying levels of light achieved the maximum-possible score.Other tests used eye charts or measured the dimmest flashes of light patients perceived in adark environment.Of the nine patients who received the maximum dosage,two had the 10,000-fold improvement in vision.“Even though we previously predicted alarge vision improvement potential in LCA1,we did not know how receptive patients’photoreceptors would be to treatment after decades of blindness,”says Cideciyan.“It is very satisfying to see asuccessful multi-center trial that shows gene therapy can be dramatically efficacious.” 查看详细>>
来源:美国宾夕法尼亚大学 点击量: 31
南京大学物理学院李绍春教授课题组在二维拓扑绝缘体研究中取得重大进展。该课题组使用精控分子束外延技术首次生长出大带隙的二维拓扑绝缘体ZrTe5单层,通过扫描隧道显微学测量发现单层ZrTe5具有不同于体结构的两种全新结构相,并存在高达~250 mV的拓扑非平庸带隙和边界金属态,为未来实现室温量子自旋霍尔效应提供了可能的材料平台。二维拓扑绝缘体存在绝缘体态和拓扑保护的导电边界态,是实现量子自旋霍尔效应的材料平台。为了在高温甚至室温下观测到量子自旋霍尔效应,需要大带隙的二维拓扑绝缘体来有效抑制体电导和热涨落。然而,目前大多数的候选材料都表现出窄带隙甚至负带隙,仅在很低的温度下才能观测到量子自旋霍尔效应。曾有理论预测表明ZrTe5单层可能是具有大带隙的拓扑绝缘体材料。然而,由于ZrTe5是相图中最不稳定的结构,且对空气非常敏感,在实验上很难获得单层ZrTe5,而通过外延方法直接生长单层ZrTe5更是面临极大的挑战。需要强调的是,单晶ZrTe5在近十年来被学术界广泛关注,很多新奇的拓扑量子现象陆续被发现。然而,由于在实验上一直未获得成功,对单层ZrTe5的拓扑性质仍然不清楚。李绍春教授课题组长期致力于二维拓扑绝缘体的实验探索。早在2016年,该课题组首次利用扫描隧道显微谱学技术证实了单晶ZrTe5为三维弱拓扑绝缘体[X.-B.Li et al.,Phys.Rev.Lett.116,176803(2016)]。随后,又利用分子束外延技术成功获得二维拓扑绝缘体单层1T’-WTe2并发现了电子相互作用的库仑能隙[Z.-Y.Jia et al.,Phys.Rev.B 96,(2017);Y.-H.Song et al.,Nat.Commun.9,4071(2018)]。然而,扫描隧道显微谱学测量显示单层1T’-WTe2具有半金属型能带(负能隙),不利于量子自旋霍尔效应的观测。最近,该课题组通过发展范德华外延方法,进一步提高了外延过程中的温度和束流精度,首次成功生长出了二维拓扑绝缘体单层ZrTe5。高分辨形貌图显示,单层ZrTe5具有两种不同于体相的新结构相(如图1),而这两种结构分别对应于面内ZrTe3三棱柱的不同排列方式(如图2)。扫描隧道显微谱显示,两种单层ZrTe5结构均具有体能隙,且高达250 meV左右。如此大的带隙满足了在室温下观测量子自选霍尔效应的要求。隧道谱学测量还显示在两种结构的边界上都具有鲁棒的一维导电边界态(如图3),通过第一性原理计算,进一步证实了如此大的能隙来源于强自旋-轨道耦合,并且这两种结构相的边界态都是拓扑非平庸的(如图4)。该发现为探索室温量子自旋霍尔效应提供了一个非常理想的材料平台。 查看详细>>
来源:南京大学 点击量: 323
A team of physicists from The University of Hong Kong(HKU),Texas Tech University(TTH),and the University of Michigan(UMich),has made an important discovery in the study of van der Waals(vdW)magnetic materials,a special class of materials with unique electronic and magnetic properties that make them attractive for use in various applications.Their research is the first to experimentally observe atransition in Nickel Phosphorus Trisulfide(NiPS3),a type of van der Waals material that has been studied for its potential applications in electronic devices and energy storage,from a3-dimensional(3D)long-range order state to a2-dimensional(2D)flat pattern vestigial order state.They have shown how the material changes its magnetic properties as it becomes thinner,revealing new insights into how this material can be used.This research is significant because it helps us understand how to control the magnetic properties of materials at very small scales,which could lead to advancements in technology,such as more efficient electronics,high-density data storage,and innovative computing devices that consume less energy.Their findings have just been published in Nature Physics and featured in‘News and Views’,highlighting its significance and implications for the field.What could we do with layered structures with just the right layers?’Richard Feynman,the Nobel Prize winner in Physics in 1965,posted this intriguing question in his famous 1959 lecture,‘Plenty of Room at the Bottom’.This statement did not receive much attention at the time,but it was revisited in the 1990s,as it was fundamentally related to the foundations of nanotechnology.In recent years,the emergence of van der Waals materials,such as NiPS3,has provided exciting opportunities for exploration of Feynman’s question.These materials consist of layers that can be easily stacked or separated,enabling researchers to investigate their properties at varying thicknesses.To address Feynman’s question,the research team turned their attention to NiPS3,which exhibits fascinating magnetic behaviour when reduced to just afew layers or even asingle layer.This unique property makes NiPS3 an ideal candidate for studying how its magnetic characteristics evolve as its thickness changes.In condensed matter physics,one of the key ways to study materials is to understand how they transition between different phases or states as their properties,like temperature or thickness change.These transitions often involve changes in the material’s symmetry,a concept known as symmetry breaking.In the case of NiPS3,the researchers observed an intermediate symmetry breaking which leads to avestigial order.Just as the term‘vestigial’refers to the retention of certain traits during the process of evolution,the vestigial order here can also be viewed as the retention during the process of symmetry breaking.This happens when the primary magnetic long-range order state melts or breaks down into asimpler form,in the NiPS3 case,a 2D vestigial order state(known as Z3 Potts-nematicity),as the material is thinned.Unlike conventional symmetry breaking,which involves the breaking of all symmetries,vestigial order only involves the breaking of some symmetries.While there are numerous examples from atheoretical standpoint,experimental realisations of vestigial order have remained challenging.However,the investigation of this 2D magnetic material has shed the first light on this issue,demonstrating that such aphenomenon can be observed through dimension crossover. 查看详细>>
来源:香港大学 点击量: 262
近日,由复旦大学工程与应用技术研究院(下文简称“工研院”)生物医学工程技术研究所常务副所长、附属华山医院放射科学术带头人耿道颖教授团队牵头研发并成功转化的科研成果“颅内动脉瘤磁共振造影图像辅助检测软件(AIneurysm)”正式获批中国国家药品监督管理局(NMPA)三类医疗器械注册证。这项重要成果的落地与转化,标志着复旦大学“医工结合”全链条创新探索取得原创性重大突破。AI加持之下,该产品将辅助医生快速、精准救治患者,提高颅内动脉瘤的诊疗效率。值得一提的是,此次获批的注册证为国内首张由高校主导、临床医生牵头研发的颅内动脉瘤磁共振AI三类医疗器械注册证,将有望为高校牵头进行同类产品的产学研研发和转化提供经验。守护人民生命健康,高水平的影像学诊断扮演着至关重要的角色,它不仅能提高疾病诊断的准确性和效率,助力早期发现和治疗,还能指导治疗方案的制定和评估疾病预后。在AI方兴未艾的时代,是否能研发一系列智能系统,学习和推广高水平医生的经验和技术,辅助提升各类疾病的诊断效率,更好地为人群服务?耿道颖团队的答案是“能”。近年来,耿道颖牵头组建了由工研院生物工程技术研究所、中科院苏州医工所及附属华山医院为骨干的智能影像医工结合团队,让临床医生、算法团队和工程师紧密结合,进行多种重大疾病智能诊断辅助系统的研发和成果转化。“颅内动脉瘤磁共振造影图像辅助检测软件”便是这支智能影像医工结合团队进行平行研发并率先落地的智能诊断辅助系统。据团队介绍,所谓颅内动脉瘤,是一种动脉壁异常膨出所形成的突起,普遍存在于全球成年人群中,动脉瘤一旦破裂即会发生急性蛛网膜下腔出血甚至破入脑实质和脑室系统,具有发病率高、致残率高、死亡率高的“三高”特点,因此又有“颅内炸弹”之称,在临床诊疗上面临着早检查、早诊断、早治疗的“三早”需求。与此同时,我国成年人群颅内动脉瘤的患病率高达7%,是欧美成年人群发病率的2-4倍,高血压糖尿病等高危人群患病率达15%左右,对颅内动脉瘤的及时诊断和治疗干预,对于急性蛛网膜下出血等脑重大疾病的预防有重要意义。据耿道颖介绍,因受限于影像设备及影像医生的水平,临床中存在着大量重大疾病误诊、漏诊等情况,针对颅内动脉瘤研发一款智能诊断辅助系统已刻不容缓。标注图像、建立AI模型、将AI模型工程化、临床测试……研发流程每个环节必须严丝合缝,在这个痛并快乐着的过程中,团队成员经历了一次次磨合,产品也经历了一次次发补材料及模型优化,而技术研发仅仅是个开始,产品在实验室出炉后,还要经过成果转化、上海检测所检测、注册前全国多中心临床试验、提交国家医疗器械审评中心审评、上海医疗器械审批中心现场体系核查等重重考验。从2019年开始立项,到2023年7月完成临床实验,再到2024年取得三类注册证,经过6年努力,团队终于走通从0到1的产学研用创新全链条,并掌握了自主研发的人工智能核心算法。作为一款人工智能产品,颅内动脉瘤磁共振造影图像辅助检测软件能辅助医生进行精准影像决策,对颅脑磁共振造影图像的显示、处理、测量和分析,对3mm及以上颅内动脉瘤辅助检测可提示疑似颅内动脉瘤患者,助力医生进行有效检测,同时量化分析动脉瘤区域,给出相关建议。“我们的产品不仅让医生的诊断效率大大提高,而且敏感性和特异性都高于医生组。”耿道颖说。据介绍,注册前全国多中心、回顾性临床试验结果表明,该软件提升动脉瘤检出率10%诊断效能由82%提高到94%,每例阅片时间缩短60%,且上手简单,3分钟即可完成培训。“希望随着产品的推广和临床应用,能提高不同地区影像医生的动脉瘤的识别水平,减轻国家、社会和家庭医疗负担,缩小不同区域和不同医院医师的阅片水平差异,让更多患者获益。”面对未来,耿道颖如是期待。 查看详细>>
来源:复旦大学 点击量: 230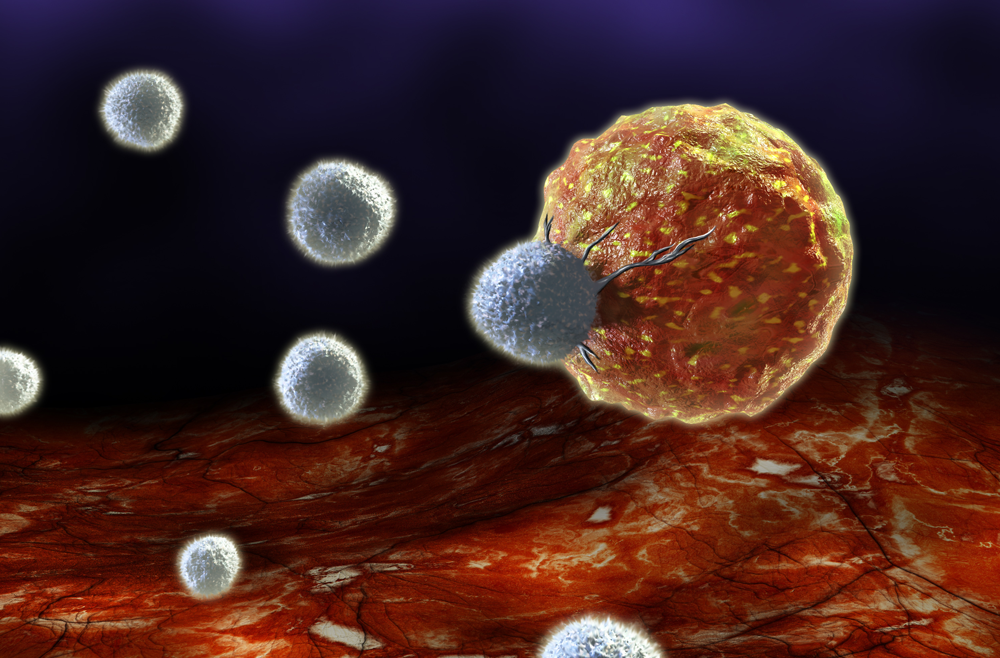
A new tool for monitoring immune health patterns over time has revealed how apair of checkpoint inhibitor therapies works together to recruit new cancer-fighting Tcells with every infusion.Findings from the use of the new tool,developed by researchers at the Perelman School of Medicine and Penn Medicine’s Abramson Cancer Center(ACC),are published in Cancer Cell.The study challenges fundamental assumptions about how acommon immunotherapy drug combination activates different types of Tcells to defeat cancer and could help researchers more precisely measure immune response in future clinical trials.Immune checkpoint inhibitors work by unleashing Tcells to find and kill cancer cells.It was thought that this type of combination immunotherapy works by equipping an army of Tcells to recognize and fight cancer throughout the course of treatment.In asense,the idea was that if this group of Tcells stayed strong for long enough,they would conquer cancer,but if they became too depleted,they would lose the battle.The study,which analyzed data from 36 patients treated with immunotherapy for advanced melanoma,found that the combination therapy produces waves of new Tcells—known as aclonal response—with each dose,rather than continually strengthening the same pool of Tcells.“We found that after every infusion,you have anew immune response,with anew group of Tcells coming in to fight the cancer,”says senior author Alexander Huang,an assistant professor of hematology-oncology and aresearch investigator with the Tara Miller Melanoma Center at the ACC.“Think about these Tcells like an army:For many cancer patients,even when they have tumors growing,experienced Tcell fighters are trying to slow down the advance of the enemy cancer cells.We call them‘exhausted Tcells’because they’ve been fighting so long,but they’re elite because they’re able to survive in ahostile environment and know how to recognize and fight the cancer cells.”To make these discoveries,the team developed anew algorithm called Cyclone to track immune response and patterns over time by following the unique receptors from individual Tcells.Looking at blood samples from the same patients,taken during different points throughout their treatment,the researchers were able to see which Tcells moved,remained,or disappeared over each patients’nine-week course of treatment.This approach also allows researchers to evaluate the magnitude of response,including how many and what type of immune cells are being activated over time as patients go through treatment.Comparatively,other current single-cell methods of studying immune response provide more of anarrow“snapshot”in time.The research team is planning to apply Cyclone in upcoming clinical trials for new cancer immunotherapy approaches,including neoadjuvant studies where Tcells can be tracked in both blood and tumor samples,and new immunotherapy combinations,such as drugs targeting PD-1 and LAG-3,a new type of checkpoint inhibitor therapy. 查看详细>>
来源:美国宾夕法尼亚大学 点击量: 27
Cognitive decline and dementia can stem from illnesses like Alzheimer’s disease and conditions like hypertension that damage blood vessels in the brain.People with both may have an even greater risk of developing cognitive impairment,a new Yale study finds.This additive effect,say researchers,will likely have an outsized impact on medically underserved populations,which makes it imperative that racially diverse trials be conducted to evaluate how to treat both contributions to dementia effectively.For the study—published Sept.4 in Alzheimer’s and Dementia:The Journal of the Alzheimer’s Association—the researchers used data from the Systolic Blood Pressure Intervention Trial,which took place between 2010 and 2015 and included adults aged 50 or older with hypertension.All told,the new study included data from 467 racially diverse trial participants aged 60 or older.wo biomarkers served as proxies for the vascular-and Alzheimer’s-related contributions to cognitive impairment.The first—white matter hyperintensity—which is abiomarker for brain scarring caused by damage to small blood vessels in the brain often due to high blood pressure,was measured via MRI when participants joined the trial.“White matter hyperintensity means that when we look at the brain via MRI,the white matter,or the nerve connections between different regions of the brain,shows up as extra white,”said Dr.Adam de Havenon,an associate professor of neurology at Yale School of Medicine and lead author of the study.“We see it as scarring of the neurons when we look at the brain during autopsies of individuals who had vascular dementia.”Alzheimer’s disease is marked by the formation of amyloid plaques,aggregates of aprotein called amyloid-beta that collect in the brain.The plaques can be seen during post-mortem analyses but can’t be directly measured non-invasively.An alternative is to measure the ratio of two peptides—Abeta42 and Abeta40—that circulate in the blood and correlate with amyloid-beta levels in the brain.The researchers evaluated which participants had scores representing the highest and lowest risks of brain scarring and amyloid plaque buildup during the first evaluation as well as who developed cognitive impairment over the following four years.“We found that the risk of developing cognitive impairment was considerably higher for the participants who had more white matter hyperintensity and more amyloid-beta than for those who just had one or the other,”said de Havenon.Specifically,the researchers found that those with the lowest risk scores for white matter hyperintensity and amyloid-beta also had the lowest rates of cognitive impairment(5.3%).Those with high scores for one risk factor but low scores for the other had higher rates of cognitive impairment(7.8%for white matter hyperintensity and 11.8%for amyloid-beta).And participants with high scores for both risk factors had the highest rates of cognitive impairment at 22.6%. 查看详细>>
来源:耶鲁大学 点击量: 207
A cancer drug that unlocks the anti-inflammatory power of the immune system could help to reduce the risk of future heart attacks,according to research part-funded by the British Heart Foundation.By repurposing an existing drug,researchers hope it could soon become part of routine treatment for patients after aheart attack.The findings will be presented at the European Society of Cardiology Congress in London by Dr Rouchelle Sriranjan,NIHR Clinical Lecturer in Cardiology at the University of Cambridge.High levels of inflammation in blood vessels are linked to an increased risk of heart disease and heart attacks.After aheart attack,the body’s immune response can aggravate existing inflammation,causing more harm and increasing risk even further.However,NICE guidelines don’t currently recommend the use of any anti-inflammatory drugs to reduce future risk.Now,a team of researchers,led by Dr Joseph Cheriyan from Cambridge University Hospitals NHS Foundation Trust,have found that low doses of an anti-inflammatory drug called aldesleukin,injected under the skin of patients after aheart attack,significantly reduces inflammation in arteries.The researchers are currently following up patients to investigate the longer-term impact of this fall in inflammation.To date,in the two and ahalf years after their treatment,there have been no major adverse cardiac events in the group that received aldesleukin,compared to seven in the group that received the placebo.Professor Ziad Mallat,BHF Professor of Cardiovascular Medicine at the University of Cambridge who developed the trial,said:“We associate inflammation with healing–an inbuilt response that protects us from infection and injury.But it’s now clear that inflammation is aculprit in many cardiovascular conditions.“Early signs from our ongoing trial suggest that people treated with aldesleukin may have better long-term outcomes,including fewer heart attacks.If these findings are repeated in alarger trial,we’re hopeful that aldesleukin could become part of routine care after aheart attack within five to 10 years.”Aldesleukin is already used to treat kidney cancer,as high doses stimulate the immune system to attack cancer cells.The Cambridge team previously found that doses one thousand times lower than those used in cancer treatment increased the number of regulatory Tcells–a type of anti-inflammatory white blood cell–in patients’blood compared to aplacebo.In the current trial at Addenbrooke‘s and Royal Papworth hospitals in Cambridge,60 patients admitted to hospital with aheart attack or unstable angina received either low dose aldesleukin or placebo.Patients received an injection once aday for the first five days,then once per week over the next seven weeks.Neither the participants nor their doctors knew whether they had received the drug or placebo.At the end of treatment,Positron Emission Tomography(PET)scans showed that inflammation in the artery involved in patients’heart attack or angina was significantly lower in the group treated with aldesleukin,compared to those who received the placebo.The anti-inflammatory effect of aldesleukin appeared even more striking in the most inflamed arteries,leading to alarger reduction in inflammation levels in these vessels and abigger difference between the two groups by the end of the study.Dr Sonya Babu-Narayan,Associate Medical Director at the British Heart Foundation and consultant cardiologist said:“Thanks to research,we have an array of effective treatments to help people avoid heart attacks and strokes and save lives.But,even after successful heart attack treatment,unwanted inflammation in the coronary arteries can remain,which can lead to life-threatening complications.“A treatment to reduce inflammation after aheart attack could be agame-changer.It would help doctors to interrupt the dangerous feedback loop that exacerbates inflammation and drives up risk.This research is an important step towards that treatment becoming areality.”The study was predominantly funded by the Medical Research Council,with significant support from the BHF and National Institute for Health and Care Research Cambridge Biomedical Research Centre(NIHR-BRC).Originally published by the British Heart Foundation. 查看详细>>
来源:剑桥大学 点击量: 723